- Jonah Duran MS, OMS-III – University Hospitals/Case Western Reserve University
- Idris Hanidu MS, MS-I – University Hospitals/Case Western Reserve University
- Chirag Soni MS, OMS-III –
- Arya Ahmady MD – University Hospitals/Case Western Reserve University
- Louis Magdon, III MD – University Hospitals
- Navkirat Bajwa MD – University Hospitals
- Christopher Furey MD – University Hospitals/Case Western Reserve University
- Nicholas Ahn MD – University Hospitals/Case Western Reserve University
ABSTRACT
Introduction
An unintentional dural tear, otherwise referred to as an incidental durotomy, is a known potential complication of spine surgery. Potential serious complications related to dural tears after spinal surgery include: pseudomeningocele, cerebrospinal fluid fistula formation, meningitis and arachnoiditis (1). However, if incidental durotomies are recognized and addressed intraoperatively, postoperative morbidity can be reduced (2). Unfortunately due to the nature of incidental durotomies, it is difficult to replicate a controlled experiment minimizing individual patient variables. Fortunately, we were able to use a similar model to Dafford and colleagues to directly compare the hydrostatic strength of dural repair techniques using various suture diameters, closure techniques, and adhesives (3); however, instead of bovine specimens, we employed a human cadaveric model.
Methods
Two balloon foley catheters were placed into the dural space, one cranially and one caudally while the balloons in each catheter were inflated to isolate the spinal segment to be tested. The caudal catheter was clamped with a hemostat, while the cranial catheter was attached to a standard IV line connected to a pressure transducer that was connected to a manometer and an IV line to a 1 L bag of Normal Saline.
The baseline leak rate was subtracted from the leak rate of the dural tear as well as the post-repair leak rate of the same cadaver to obtain both the corrected dural tear leak rate and the corrected post-repair leak rate. The percent change in leak rate was obtained for each cadaver, each suture type, and each suture technique and then analyzed using a paired two tailed t-test (p=0.05).
Results
In total, there were 16 cadavers included in the analysis all using prolene suture. Among the groups, there were 4 samples using 6-0 prolene repaired with simple interrupted sutures, 4 samples of 6-0 prolene repaired with running suture, 4 samples of 5-0 prolene repaired with simple interrupted sutures, and 4 samples of 5-0 prolene repaired with running suture. Of note, the percent change in leak rate post-repair in the 5-0 prolene interrupted group was notably larger than that of the 6-0 prolene interrupted and 6-0 prolene running; however, the differences were not statistically significant (p=0.155 and 0.105, respectively).
Conclusion
Overall, we found that there were no significant differences between using a 5-0 vs 6-0 prolene suture as well as no significant differences between using simple interrupted or simple running suture. Further directions this study could undergo would be to determine the difference between using nylon vs prolene suture or the efficacy of using fibrin glue or fat patch repair. Despite its limitations, this model can be used as a building block to better study various dural repair techniques.
References
- Goodkin R, Laska LL (1995) Unintended ‘‘incidental’’ durotomy during surgery of the lumbar spine: medicolegal implications. Surg Neurol 43:4–12.
- Alexander A, Jones M, Stambough JL et al (1989) Long-term results of lumbar spine surgery complicated by unintended incidental durotomy. Spine 14(4):443–446.
- Doherty, C. M., & Forbes, R. B. (2014). Diagnostic Lumbar Puncture. The Ulster medical journal, 83(2), 93–102.
Keywords
Durotomy, repair, human cadaver, spine
MANUSCRIPT
Introduction
An unintentional dural tear, otherwise referred to as an incidental durotomy, is a known potential complication of spine surgery for degenerative cervical, lumbar, and thoracic disease. Although the incidence of incidental durotomies varies according to the region of the vertebral column being operated on, several studies have reported varying findings. In a retrospective analysis of 361 patients, Grewal and his colleagues report a dural tear rate of 7.8% with lumbar surgery compared with 1.4% cervical and 3.8% thoracic [1]. In a larger study involving 13,188 patients with degenerative lumbar diseases who underwent primary lumbar spine surgery, the rate of dural tears was reported to be 3.4% [2]. A 10 year systematic literature review of 19 studies (comprising 15,965 patients) revealed an overall durotomy rate of 8.11% (range 2%–20%) for open approach lumbar surgeries [3], which is similar to a study reporting the rate of dural tears in patients treated for adult spinal deformities as being 10.8% [4].
Regardless of the incidence of incidental durotomies, several studies have reported them to be associated with a statistically significantly higher rate of complications such as surgical site infections, post-operative neurological deficits, and post-operative delirium [2]. Prior studies have revealed other potentially serious complications including pseudomeningocele, cerebrospinal fluid fistula formation, meningitis, and arachnoiditis all related to dural tears and CSF leakage after spinal surgery [5]. However, if incidental durotomies are recognized and addressed intraoperatively, post-operative morbidity can be reduced [6]. One long term study demonstrated that dural tears that were immediately recognized and treated accordingly did not lead to any significant sequelae at a mean follow-up of 37 months [7].
In regards to which dural repair techniques to employ and the outcomes of each technique used to address an incidental durotomy, much research has been done to address this question. One retrospective study examining intraoperative dural tears among patients undergoing lumbar pedicle subtraction osteotomy for ankylosing spondylitis used a direct repair with 4-0 silk sutures for small dural tears, while larger ones were repaired with muscle, fascia, or fat grafts harvested from the adjacent operation site. No complications were noted in either group, other than one patient who experienced a malfunction of the intraoperatively placed lumbar drain [8]. Another retrospective review of patients undergoing degenerative spinal and spine tumor surgery addressed any dural tears in 51 patients with either fibrin glue, surgicel and fibrin glue, and running locked suture with or without fibrin glue or surgicel. They found that 13 out of 51 of the repaired patients presented afterwards with a postoperative complication, and 9 out of 13 resulted in a revision procedure [7]. Among seven patients undergoing microendoscopic laminotomy, one study reported the use of a polyglactin sheet cut into small squares between 3 mm and 10 mm in , then soaked in fibrinogen and placed over the dural tear, with several drops of thrombin placed over the patch [9]. The use of fat grafts harvested from patients’ subcutaneous layer has been studied as well. The advantages of the use of fat grafts are that they are impervious to water, cause little scarring, and can prevent CSF from seeping around the fat [10]. The same study reported the use of fibrin glue spread on the surface of the fat that is further covered with Surgicel or Gelfoam, and the repair of ventral dural tears with a large fat graft packed loosely to fill the disc space [10]. Lastly, one study compared the outcomes of 69 dural tears repaired with either a sole dural suture, a patch (comprised of either TachoSil, muscle, or fat), or a dural suture in combination with a patch. The authors reported that the 3 groups showed no significant difference in rates of revision surgery, as well as no difference in hospitalization time, operation time, or clinical outcome [11]. Another study achieved similar results, demonstrating no significant difference in outcome between varying methods of dural repair [1].
Despite the studies demonstrating new techniques and patient outcomes, little research has been done in directly evaluating the strength and leak rate in an in vitro model. Unfortunately, due to the nature of incidental durotomies, it is difficult to replicate a controlled experiment minimizing individual patient variables. Fortunately, a recent study from Dafford and colleagues introduced the development of a model that can be used to directly compare the hydrostatic strength of dural repair techniques using various sutures, closure techniques, and adhesives [12]. The authors used T11-L5 portions of calf spines, which had two 14 French two-way Foley catheters placed into the dural space, one cranially and one caudally. The caudal one was clamped with a hemostat, while the cranial Foley catheter was connected to a reservoir of normal saline via continuous bladder irrigation tubing and a drip chamber.
Raising or lowering the reservoir increased/decreased the pressure in the dura, while the balloons in each catheter were inflated to isolate the spinal segment to be tested. Their results demonstrated that 6-0 Prolene was found to have significantly decreased leakage flow rate than 5-0 surgilon; however, they found no significant differences in the flow rate between the interrupted and continuous locked sutures. Furthermore, they demonstrated an 80% reduction in leak area with the hydrogel and cyanoacrylic sealants compared with only a 38% reduction with fibrin glue [12]. Using a similar model, we intend to employ a similar design to determine the direct outcomes of various dural repair techniques; however, we will employ a human cadaveric model.
Materials and Methods
Setup
Human cadavers were obtained from Case Western Reserve University School of Medicine Department of Anatomy with the experiment taking place in the Anatomy Laboratory of the School of Medicine. The cadavers were placed in the prone position, and a midline incision with dissection was used to expose the spine. The lamina was removed exposing the dural sac. Two midline incisions were made with a 10-blade scalpel: one cranial to the region of interest and one caudal. One balloon foley catheter (BARDEX IC®) was placed at each end of the dural of the segment where the incisions were made and inflated with normal saline. The caudal catheter was clamped with a hemostat, while the cranial catheter was attached to a standard IV line connected to a pressure transducer with two 3-way stopcocks (Transpace® IV Monitoring Kit, 60”, 03ml Squeeze Flush Device, 2 3-Way Stopcocks and Macrodrip).
To measure the pressure within the system, a standard lumbar puncture kit was used (PresourceTM STRL Lumbar Puncture 20Gx3 5). A two-piece manometer was placed in the top hole of the transducer to measure the pressure inside the system (Figure 1). One end of the pressure transducer was connected via standard IV line to the cranial foley catheter in the cadaver, while the other end of the transducer was connected via an IV line to a 1 L bag of Normal Saline suspended by an IV pole.

Determining Baseline Leak Rate
Upon completion of the setup, the normal saline was allowed to flow within the system to reach a pressure of 21 cm H2O on the manometer, a value that reflects a normal physiological opening pressure [13]. The height of the IV bag of normal saline was adjusted to obtain this value. Once this value was achieved, the system was then allowed to run for 2 minutes, after which the stopcock was closed, and any additional fluid was prevented from entering the system. At this point, any normal saline that was present outside the dura was collected via a 10cc syringe and measured in a 200 mL beaker. The amount of fluid collected prior to any durotomy is referred to as the baseline leak rate. To account for variability between each cadaver, the baseline leak rate for each cadaver was determined separately.
Determining Leak Rate Post Durotomy and Repair
After the baseline leak rate was determined, a standard scalpel with a 10-blade was used to make a 1 cm incision in the dura at the lumbar level to mimic an incidental durotomy. With the pressure in the manometer maintained at 21 cm H2O, a timer was started and exactly 120 seconds were allowed to pass before the stopcock was closed to prevent any fluid from entering the system. As before, any normal saline that was present outside the dura was then collected via a 10cc syringe and measured in a 200 mL beaker.
The repairs were performed using various suture types and techniques. The suture types used were 6-0 Prolene (Ethicon TM) and 5-0 Prolene (Ethicon TM). With each suture type, several techniques were employed; these included simple running and simple interrupted. To ensure minimal variability in the repairs themselves, each repair was performed by an orthopaedic spine surgery fellow or attending. After the repair was performed, the leak rate was determined by restarting the flow of normal saline into the system, while maintaining the pressure at the same level as the pre-repair and dural tear (Figure 2). After exactly 120 seconds, the shuttlecock was turned into the off position and normal saline was prevented from entering the system. Once again, any normal saline that was present outside the dura was then collected via a 10cc syringe and measured in a 200 mL beaker.
The repairs were performed using various suture types and techniques. The suture types used were 6-0 Prolene (Ethicon TM) and 5-0 Prolene (Ethicon TM). With each suture type, several techniques were employed; these included simple running and simple interrupted. To ensure minimal variability in the repairs themselves, each repair was performed by an orthopaedic spine surgery fellow or attending. After the repair was performed, the leak rate was determined by restarting the flow of normal saline into the system, while maintaining the pressure at the same level as the pre-repair and dural tear (Figure 2). After exactly 120 seconds, the shuttlecock was turned into the off position and normal saline was prevented from entering the system. Once again, any normal saline that was present outside the dura was then collected via a 10cc syringe and measured in a 200 mL beaker.

Analysis
To analyze the data, each cadaver was analyzed separately. Once the baseline leak rate of an individual cadaver was calculated, it was subtracted from the leak rate of the dural tear as well as the post-repair leak rate of the same cadaver to obtain both the corrected dural tear rate and the corrected post-repair rate. The corrected post-repair leak rate was subtracted from the corrected dural tear leak rate, which was then divided by the corrected dural tear leak rate to obtain a value referred to as the percent change in leak rate. The percent change in leak rate was obtained for each cadaver, each suture type, and each suture technique and then analyzed using a paired two tailed t-test (significance 0.05).
Results
In total, there were 16 cadavers included in the analysis, all using prolene suture. Among the groups, there were 4 samples using 6-0 prolene repaired with simple interrupted sutures, 4 samples of 6-0 prolene repaired with running suture, 4 samples of 5-0 prolene repaired with simple interrupted sutures, and 4 samples of 5-0 prolene repaired with running suture. When the needle of sutures were compared (5-0 vs 6-0 prolene) independent of suture technique, the percent change in the tear rate when 6-0 prolene was used was 80.73% (standard error 13.08), while 5-0 prolene was 97.58% (standard error 29.94), with no significant difference between the two rates (p=0.737) as seen in Figure 3. When the suture technique was compared independent of needle , the percent change in the tear rate when a simple interrupted suture was used was 89.82% (standard error 31.72%), while a running suture was 91.11% (standard error 7.64), with no significant difference between the two rates as well (p=0.836) as seen in Figure 3. Lastly, when each type of suture repair and needle were compared, there were no significant differences between each group as noted by the p values in table 1. Of note, the percent change in leak rate post repair in the 5-0 prolene interrupted group was notably larger than that of the 6-0 prolene interrupted and 6-0 prolene running; however, the differences were not statistically significant (p=0.155 and 0.105 respectively).
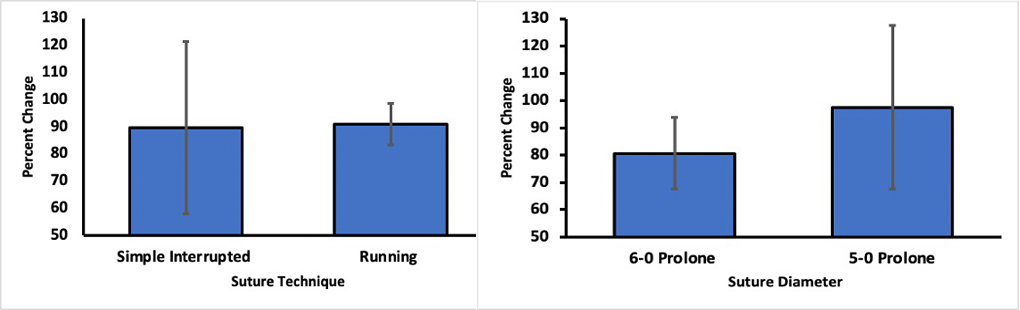
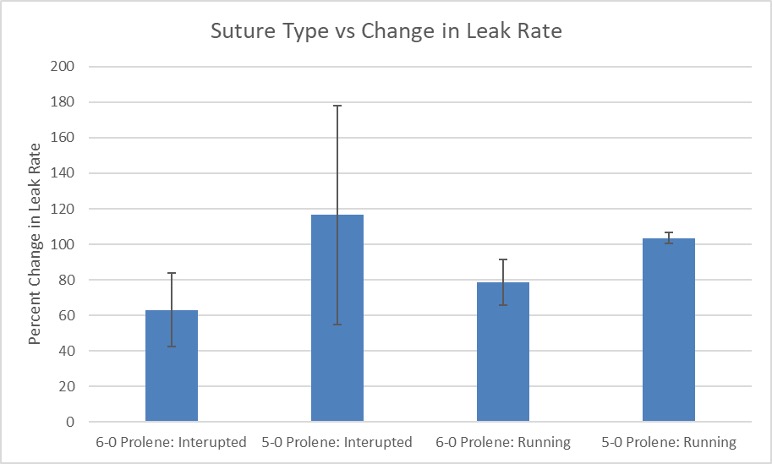
Table 1: p-values of various suture techniques and suture diameters when compared against each other
| 5-0 Prolene: Interrupted | 5-0 Prolene: Running | 6-0 Prolene: Running | |
| 6-0 Prolene: Interrupted | 0.557 | 0.615 | 0.155 |
| 5-0 Prolene: Interrupted | 0.551 | 0.649 | |
| 5-0 Prolene: Running | 0.105 |
Note: Significance to the nearest thousandth
Discussion
To determine the differences in various dural repair techniques, we developed a human cadaver model that can be used to test the strength of different sutures and techniques in regards to closures of durotomies. Our model utilizes many of the same aspects as that developed by Dafford and colleagues, however it attempts to do so in human physiological conditions. We attempted to determine how altering suture and technique would have an effect on the leak rate after a dural repair. Overall, we found that there were no significant differences between using a 5-0 vs 6-0 prolene suture as well as no significant differences between using simple interrupted or simple running suture. These findings seem to correlate with those found by Dafford colleagues; however, we were not able to procure enough cadavers to examine how nylon sutures or the use of fibrin glue would affect suture strength.
Despite the insight that can be gained from using this model, this study does have some limitations. Of note, the cadavers used in this experiment were fixed with formaldehyde rather than being fresh frozen cadavers, thus they are not able to exactly replicate living human tissue. Furthermore, fixation differed from cadaver to cadaver, thus the quality and consistency of the dural tissue used varied considerably. Therefore, the various repair techniques and materials used might have different results in a more in vivo model. Additionally, 0.9% normal saline was used in place of cerebrospinal fluid, which has a different composition and consistency than human cerebrospinal fluid. The measurement of the exact amount of fluid that leaked from the repair was determined using 10cc syringes, thus we were not able to account for any fluid that may have been absorbed by surrounding tissues. Lastly, the limited number of cadavers used in this study proved to be a significant factor in our statistical analysis. To keep the dural tears at the same level and preserve the integrity of the dural tissue, we limited one trial of dural tear and repair per cadaver. This may have recreated a more in vivo situation; however, it decreased the number of trials we could obtain in this study.
Conclusion
Overall, we found that there were no significant differences between using a 5-0 vs 6-0 prolene suture as well as no significant differences between using simple interrupted or simple running suture. Further directions this study could undergo would be to determine the difference between using nylon vs prolene suture or the efficacy of using fibrin glue or fat patch repair. Despite its limitations, this model can be used as a building block to better study various dural repair techniques.
References
- Grewal, I. S., Grewal, U. S., Eadsforth, T., Barrett, C., & Pillay, R. (2019). Incidence and Management of Incidental Spinal Durotomies Noticed During Spinal Surgery. The Open Orthopaedics Journal, 13(1).
- Takenaka, S., Makino, T., Sakai, Y., Kashii, M., Iwasaki, M., Yoshikawa, H., & Kaito, T. (2019). Dural tear is associated with an increased rate of other perioperative complications in primary lumbar spine surgery for degenerative diseases. Medicine, 98(1).
- Ghobrial, G. M., Theofanis, T., Darden, B. V., Arnold, P., Fehlings, M. G., & Harrop, J. S. (2015). Unintended durotomy in lumbar degenerative spinal surgery: a 10-year systematic review of the literature. Neurosurgical focus, 39(4), E8.
- Iyer, S., Klineberg, E. O., Zebala, L. P., Kelly, M. P., Hart, R. A., Gupta, M. C., … & Smith, J. S. (2018). Dural tears in adult deformity surgery: incidence, risk factors, and outcomes. Global spine journal, 8(1), 25-31.
- Goodkin R, Laska LL (1995) Unintended ‘‘incidental’’ durotomy during surgery of the lumbar spine: medicolegal implications. Surg Neurol 43:4–12.
- Alexander A, Jones M, Stambough JL et al (1989) Long-term results of lumbar spine surgery complicated by unintended incidental durotomy. Spine 14(4):443–446.
- Guerin, P., El Fegoun, A. B., Obeid, I., Gille, O., Lelong, L., Luc, S., … & Vital, J. M. (2012). Incidental durotomy during spine surgery: incidence, management and complications. A retrospective review. Injury, 43(4), 397-401.
- Jo, D.-J., Kim, K.-T., Lee, S.-H., Cho, M.-G., & Seo, E.-M. (2015). The Incidence and Management of Dural Tears and Cerebrospinal Fluid Leakage during Corrective Osteotomy for Ankylosing Spondylitis with Kyphotic Deformity. Journal of Korean Neurosurgical Society, 58(1), 60–64. http://doi.org/10.3340/jkns.2015.58.1.60.
- Shibayama, M., Mizutani, J., Takahashi, I., Nagao, S., Ohta, H., & Otsuka, T. (2008). Patch technique for repair of a dural tear in microendoscopic spinal surgery. Bone & Joint Journal, 90(8), 1066-1067.
- Black, P. (2002). Cerebrospinal fluid leaks following spinal surgery: use of fat grafts for prevention and repair. Journal of Neurosurgery: Spine, 96(2), 250-252.
- Kamenova, M., Leu, S., Mariani, L., Schaeren, S., & Soleman, J. (2016). Management of incidental dural tear during lumbar spine surgery. to suture or not to suture?. World neurosurgery, 87, 455-462.
- Dafford, E. E., & Anderson, P. A. (2015). Comparison of dural repair techniques. The Spine Journal, 15(5), 1099-1105.
- Doherty, C. M., & Forbes, R. B. (2014). Diagnostic Lumbar Puncture. The Ulster medical journal, 83(2), 93–102.
Required Disclosures and Declaration
Copyright Information: No Copyright Information Added
IRB Approval Information: Yes
Disclosure Information: No known conflicts of interest


